Ulcer as the only manifestation of disseminated cryptococcosis in a patient with rheumatoid arthritis
DOI:
https://doi.org/10.47196/da.v31i2.2875Keywords:
extrapulmonary cryptococcosis, cutaneous cryptoccocosis, non HIV immunosuppressionAbstract
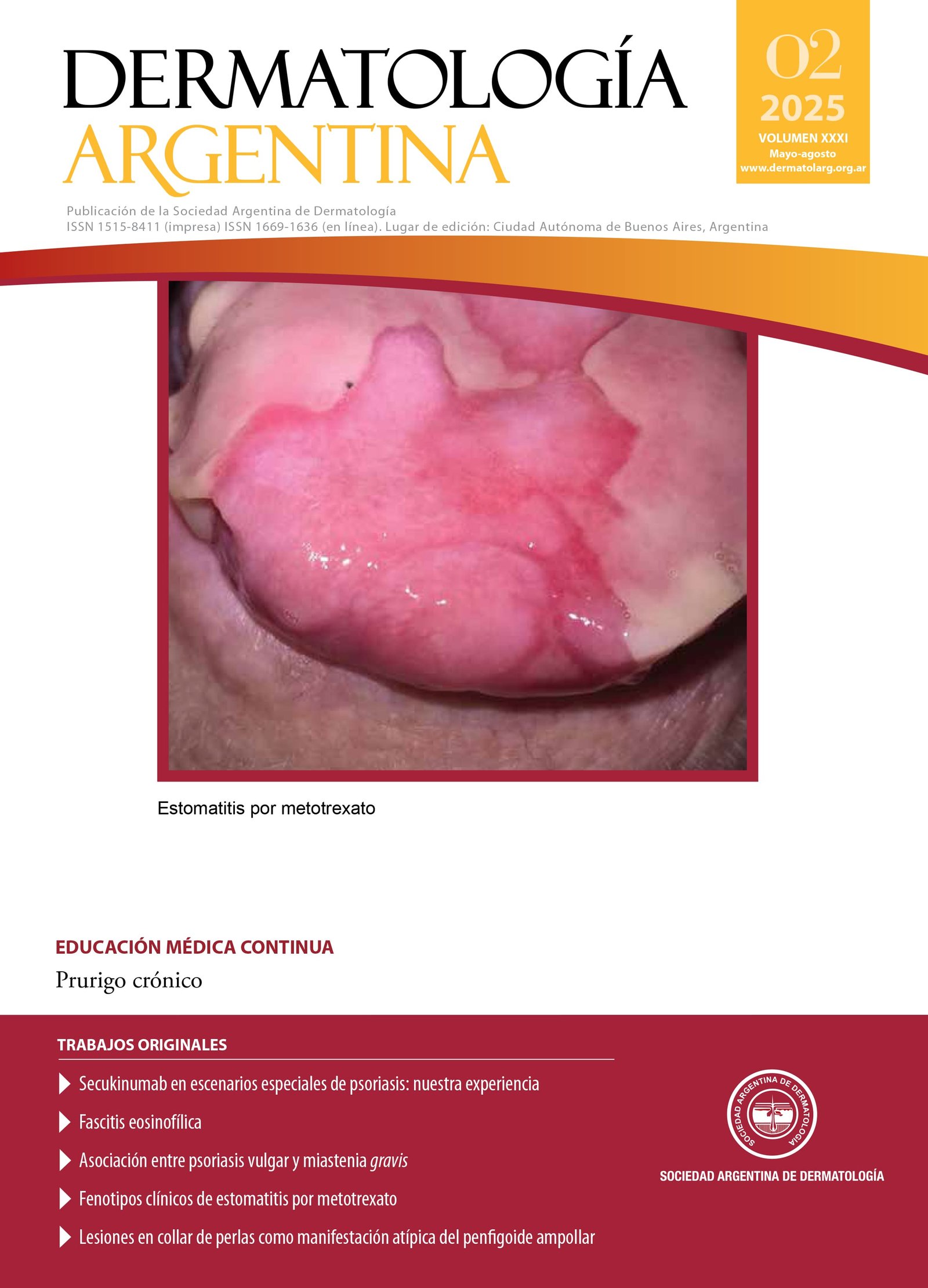
Cryptococcosis is a systemic mycosis caused by yeasts of the genus Cryptococcus. Extrapulmonary forms are frequently observed in patients with immunodeficiencies. Skin lesions are characterized by clinical polymorphism, presenting molluscoid papules, pustules, subcutaneous abscesses, nodules and acneiform lesions. Ulcer as a clinical manifestation is rare. Diagnosis is established through direct visualization of the fungus and cultures. The first-line treatment is amphotericin B and in mild forms fluconazole may be indicated. We present the exceptional case of a patient with rheumatoid arthritis being treated with glucocorticoid, methotrexate and leflunamide who presented an ulcer as the only manifestation of disseminated cryptococcosis.
References
I. Negroni R. Cryptococcosis. Clin Dermatol. 2012;30:599-609.
II. Gushiken AC, Saharia KK, Baddley JW. Cryptococcosis. Infect Dis Clin North Am. 2021;35:493-514.
III. Trillos RF, et ál. Meningoencefalitis criptococócica en una paciente con artritis reumatoide tratada con metotrexato y prednisona. Reumatol Clin. 2014;10:346-347.
IV. Arechavala A, et ál. Cryptococcosis in an infectious diseases hospital of Buenos Aires, Argentina. Revision of 2041 cases. Diagnosis, clinical features and therapeutics. Rev Iberoam Micol. 2017;35:1-10.
V. Bordel MT, Zafra MI, Cardeñoso-Álvareza ME, Sánchez-Estella J, et ál. Celulitis necrotizante como primera manifestación de una criptococosis diseminada. Actas Dermosifiliogr. 2011;102:297-307.
VI. Lin YY, Shiau S, Fang CT. Risk factors for invasive Cryptococcus neoformans diseases: a case-control study. PLoS One. 2015;10:1-13.
VII. Olivares L, Gagliardi M, Fischer J, Maronna E, et ál. Criptococosis cutánea símil pioderma gangrenoso en paciente inmunosuprimido no VIH. Dermatol Argent. 2016;22:40-43.
VIII. Bratton EW, Husseini N, Chastain CA, Lee MS, et ál. Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIV-negative/non-transplant. PLoS One. 2012;7:1-10.
IX. Messina F, Santiso G, Arechavala A, Romero M, et ál. Preemptive therapy in Cryptococcosis adjusted for outcomes. J Fungi (Basel). 2023;9:631.
X. Kothiwala SK, Prajapat M, Kuldeep CM, Jindal A. Cryptococcal panniculitis in a renal transplant recipient: case report and review of literature. J Dermatol Case Rep. 2015;30:76-80.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 on behalf of the authors. Reproduction rights: Argentine Society of Dermatology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor