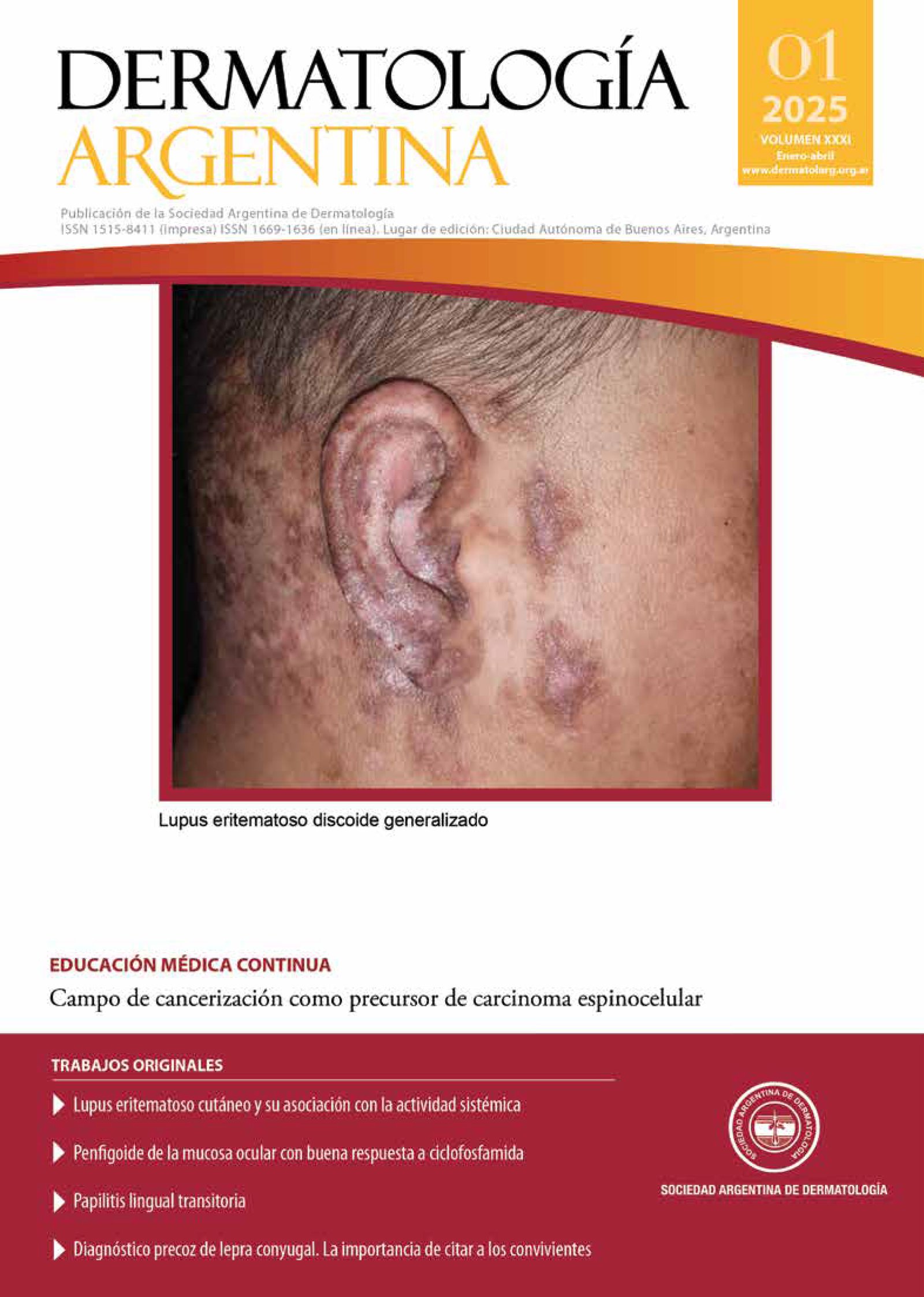
Cutaneous lupus erythematosus and its association with systemic activity
DOI:
https://doi.org/10.47196/da.v31i1.2653Keywords:
cutaneous lupus erythematosus, systemic lupus erythematosusAbstract
Background: systemic lupus erythematosus (SLE) is an autoimmune disease with multiorgan involvement that can affect the skin. There is limited data on the association between skin involvement and systemic disease activity.
Objectives: to describe the different clinical variants of cutaneous lupus erythematosus (CLE) in our population and identify the association with SLE and its activity, severity, and the organs and systems involved.
Design: retrospective cross-sectional study.
Materials and methods: patients aged ≥15 years with SLE and/or CLE who attended the dermatology department of Hospital Interzonal General de Agudos San Martín (La Plata), between March 2015 and April 2024 were included. The first consultation for each cutaneous manifestation was recorded.
Results: a total of 93 consultations from patients with SLE and/or CLE were recorded, of which 85 were women and 8 were men. In 67 cases, patients presented cutaneous manifestations of lupus erythematosus. The group with simultaneous specific and nonspecific lesions and the group with three or more distinct skin lesions were statistically associated with disease activity, specifically with a moderate severity level, and were mainly linked to alopecia, hypocomplementemia, anti-dsDNA, and oral ulcers, without an association with organ involvement.
Conclusions: the simultaneous presence of nonspecific and specific skin lesions, as well as 3 or more types of skin lesions, was associated with an increase in the systemic activity of the disease. These findings warrant prospective studies with a larger number of patients.
References
I. Vale ECS, García LC. Cutaneous lupus erythematosus: a review of etiopathogenic, clinical, diagnostic and therapeutic aspects. An Bras dermatol. 2023;98:355-372.
II. Gladman DD, Ibáñez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29:288-291.
III. Fanouriakis A, Kostopoulou M, Andersen J, Aringer M, et ál. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann Rheum Dis. 2024;83:15-29.
IV. Yee CS, Farewell VT, Isenberg DA, Bridget G, et ál. The use of Systemic Lupus Erythematosus Disease Activity Index-2000 to define active disease and minimal clinically meaningful change based on data from a large cohort of systemic lupus erythematosus patients. Rheumatology. 2011;50:982-988.
V. Cooper EE, Pisano CE, Shapiro SC. Cutaneous manifestations of “lupus”: systemic lupus erythematosus and beyond. Int J Rheumatol. 2021;1-19.
VI. Consenso sobre lupus eritematoso cutáneo. Actualización 2016. Sociedad Argentina de Dermatología. Buenos Aires, Argentina. 2016. Disponible en: https://sad.org.ar/wp-content/uploads/2019/10/LUPUS-FINAL-07122016.pdf.
VII. Gilliam JN, Sontheimer RD. Distinctive cutaneous subsets in the spectrum of lupus erythematosus. J Am Acad Dermatol. 1981;4:471-475.
VIII. Zeĉević RD, Vojvodić D, Ristić B, Pavlović MD, et ál. Skin lesions-an indicator of disease activity in systemic lupus erythematosus? Lupus. 2001;10:364-367.
IX. Petri M, Orbai AM, Alarcón GS, Gordon C, et ál. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64:2677-2686.
X. Aringer M, Costenbader K, Daikh D, Brinks R, et ál. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2019;71:1400-1412.
XI. Zambernardi A, Bendjuia G, Manzano RE, Berben MD, et ál. Lupus eritematoso cutáneo. Estudio de 92 pacientes. Dermatol Argent. 2018;24:41-46.
XII. Ortega SM, Barbarulo A, Spelta M, Gavazza S, et ál. Lupus eritematoso cutáneo: revisión de nuestra casuística en los últimos 15 años. Dermatol Argent. 2011;17:116-122.
XIII. Cosentino M, Martire MV, García L, García MA, et ál. Manifestaciones cutáneas en pacientes con lupus eritematoso sistémico: formas al inicio de la enfermedad y durante el seguimiento. Análisis retrospectivo. Reumatol Clin. 2023;19:293-298.
XIV. Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: issues in diagnosis and treatment. Am J Clin Dermatol. 2009;10:365-81.
XV. Contestable JJ, Edhegard KD, Meyerle JH. Bullous systemic lupus erythematosus: a review and update to diagnosis and treatment. Am J Clin Dermatol. 2014;15:517-524.
XVI. Concha JSS, Werth VP. Alopecias in lupus erythematosus. Lupus Sci Med. 2018;5:e000291.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 on behalf of the authors. Reproduction rights: Argentine Society of Dermatology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor