Mucous membrane pemphigoid through the years in our Department
DOI:
https://doi.org/10.47196/da.v27i4.2223Keywords:
Mucous membrane pemphigoid, cicatricial pemphigoid, ocular pemphigoidAbstract
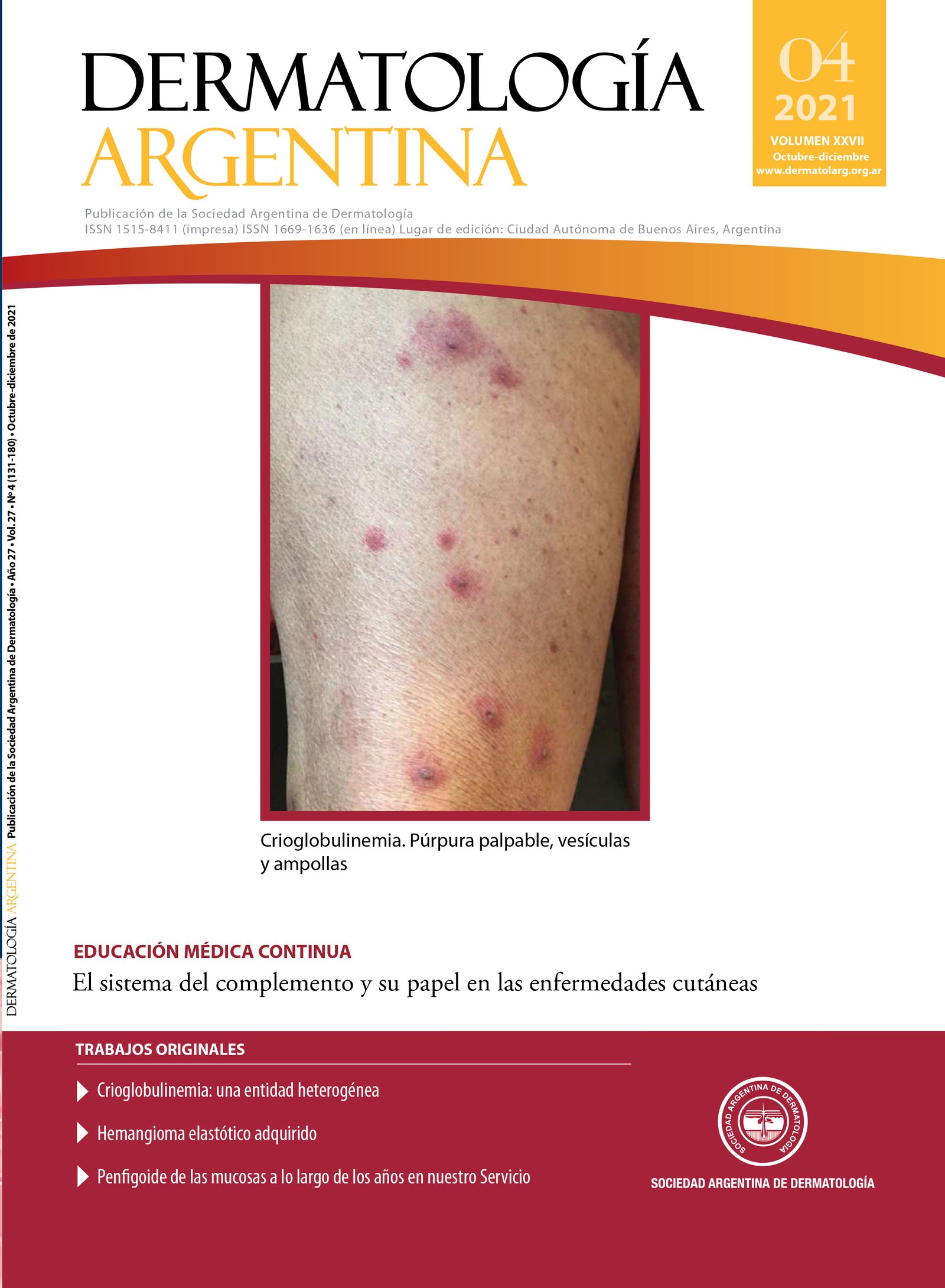
Introduction: mucous membrane pemphigoid (MMP), also known as benign mucous membrane pemphigoid, cicatricial or mucosynechial pemphigoid, belongs to an heterogeneous group of chronic in ammatory autoimmune blistering diseases, which involves the mucous membranes (oral, ocular, pharyngeal, nasal, esophageal, laryngeal and anogenital) and/ or skin with tendency to scar formation.
There are autoantibodies against di erent components of the basement membrane zone (BPAG 1- BPAG2, Integrin α6β4, Laminin 332, Col VII, among others). The direct immunofluorescence (DIF) will be of paramount importance, as well as the clinical diagnosis.
Objective: review the cases diagnosed with mucous membrane pemphigoid for 24 years (January 1997- March 2021) in the Blistering Disease Clinic at the Dermatology Department at the Ramos Mejia Hospital to establish the epidemiologic, clinic presentation and available treatments in this pathology.
Design: retrospective descriptive and observational study of the clinical and immunopathological characteristics of 34 patients with MMP that were treated at the Blistering Disease Clinic at the Dermatology Department at the Ramos Mejia Hospital between January 1997 and March 2021.
Materials and methods: though the medical histories and the photographic registries, we evaluated the following variables: prevalence of MMP within the patients that came to consult at the
Blistering Disease Clinic at the Dermatology Department, sex, age, personal history, the a ected mucous, evolution time until the diagnosis, direct immuno uorescence findings, clinical follow-ups and treatments.
Results: we studied the clinical evolution of 34 patients diagnosed with MMP at our institution (5.3% from the total of patients at the Blistering Disease Clinic).The most a ected gender was female and the average age at diagnosis was 64 years. 70.6% presented comorbidities such as hypertension and hypothyroidism. Most of our patients referred an emotional triggering event. The most affected membrane mucous was the ocular one and the oral was the second one. The delay in diagnosis was 4 years and 11 months. Linear deposits of IgG was the most frequent result in the direct immunofluorescence. 17.6% did not continue clinical follow-up. Mycophenolate mofetil was the most used drug with a good therapeutic response.
Conclusions: MMP is a rare autoimmune disease that affects mucous membrane and occasionally the skin. In this study, the ocular involvement was the most frequent one, di ering with the international reports. The early interdisciplinary diagnosis is essential to avoid irreversible sequelae.
References
I. Tula M. Penfigoide de las mucosas. Dermatol Argent. 2012;18:16-23.
II. Giuli Santi C, Gripp AC, Roselino AM, Santana Mello D, et ál. Consensus on the treatment of autoimmune bullous dermatosis: bullous pemphigoid, mucous membrane pemphigoid and epidermolysis bullosa acquisita - Brazilian Society of Dermatology. An Bras Dermatol. 2019;4:33-47.
III. Broussard KC, Leung TG, Moradi A, Thorne JE, et ál. Autoimmune bullous diseases with skin and eye involvement: cicatricial pemphigoid, pemphigus vulgaris and pemphigus paraneoplastica. Clin Dermatol. 2016;34:205-213.
IV. Lee J, Seiffert-Sinha K, Attwood K, Sinha AA. A Retrospective Study of Patient-Reported Data of Bullous Pemphigoid and Mucous Membrane Pemphigoid from a US-Based Registry. Front Immunol. 2019;10:2219.
V. Madgar O, Baniel A, Yarom N, Glikson E, et ál. Mucous membrane pemphigoid–otorhinolaryngological manifestations: a retrospective cohort study. Eur Arch Otorhinolaryngol. 2020;277:939-945.
VI. López Gamboa VR, Castaño MB, Videla I, Rossello VE, et ál. Penfigoide cicatrizal ocular. Dermatol Argent. 2018;24:128-132.
VII. Kamaguchi M, Iwata H. The diagnosis and blistering mechanisms of mucous membrane pemphigoid. Front Immunol.2019;10:1-8.
VIII. Buonavoglia A, Leone P, Dammacco R, Di Lernia G, et ál. Pemphigus and mucous membrane pemphigoid: An update
from diagnosis to therapy. Autoimmun Rev. 2019;18:349-358.
IX. Forero OL, Candiz ME, Fernández Bussy R, Dickson C, et ál. Guías de manejo de penfigoide ampollar 2021 [en línea]. Publicación de la Sociedad Argentina de Dermatología, julio 2021;1(1). Disponible en: <https://sad.org.ar/wp-content/uploads/2021/09/Guias-de-
manejo-de-PA.pdf> [Consultado septiembre 2021].
X. Daluvoy MB, Valenzuela FA, Pérez VL. Mucous membrane pemphigoid. En: Mannis M, Holland E. Cornea. 5th ed. Londres: Elsevier; 2021:549-558.
XI. Anesi SD, Eggenschwiler L, Ferrara M, Artornsombudh P, et ál. Reliability of conjunctival biopsy for diagnosis of ocular mucous membrane pemphigoid: redetermination of the standard for diagnosis and outcomes of previously biopsy- negative patients. Ocul Immunol Inflamm. 2020;4:1-8.
XII. Candiz ME, Forero O, Olivares L, Muñoz del Toro M, et ál. Diagnóstico serológico de patologías ampollares autoinmunitarias. Dermatol Argent. 2018;24:177-184.
XIII. Hong GH, Khan IR, Shifera AS, Chinwenwa O, et ál. Incidence and clinical characteristics of ocular involvement in mucous membrane pemphigoid. Ocul Immunol Inflamm. 2019;27:821-825.
XIV. Ali S, Kelly C, Challacombe SJ, Donaldson ANA, et ál. Salivary IgA and IgG antibodies to bullous pemphigoid 180 noncollagenous domain 16a as diagnostic biomarkers in mucous membrane pemphigoid. Br J Dermatol Suppl. 2016;174:1022-1029.
XV. Chiganera EH, Albera P. Penfigoide ocular cicatricial: hallazgos de biopsia conjuntival y su relación con la inflamación y cicatrización ocular. Rev Mex Oftalmol. 2016;91:134-141.
XVI. Patel MP, Jones VA, Murray TN, Amber KT. A Review Comparing International Guidelines for the Management of Bullous Pemphigoid, Pemphigoid Gestationis, Mucous Membrane Pemphigoid, and Epidermolysis Bullosa Acquisita. Am J Clin Dermatol 2020;21:557-565.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Argentine Society of Dermatology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor