Cryoglobulinemia: a heterogeneous entity
DOI:
https://doi.org/10.47196/da.v27i4.2219Keywords:
cryoglobulinemia, cryoglobulins, vasculitis, cryoglobulinemic syndromeAbstract
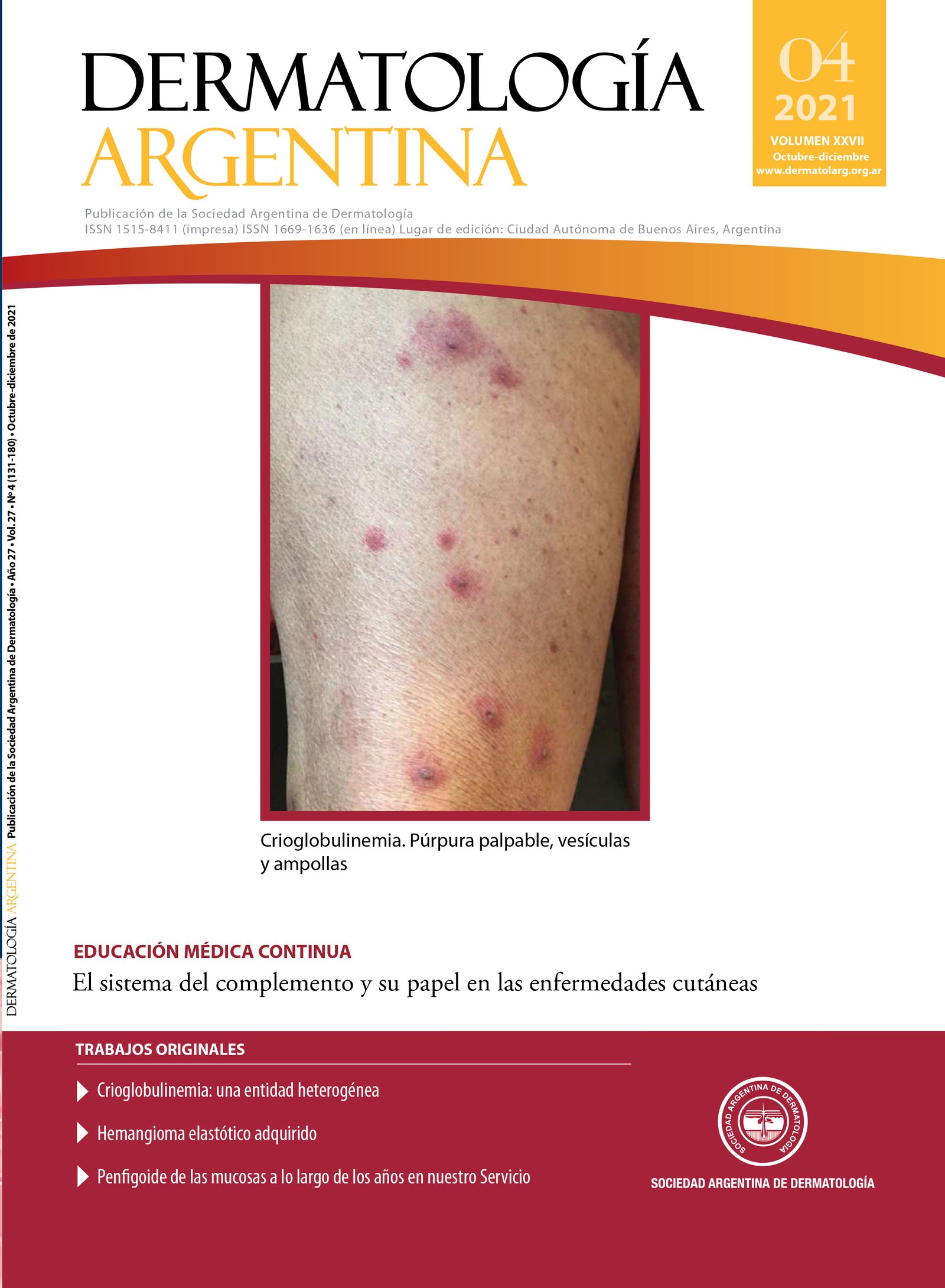
Cryoglobulinemia is defined as the presence of immunoglobulins in serum that reversibly precipitate at low temperatures. It is classified into types I, II and III on the basis of immunoglobulin characteristics. Type I is associated with lymphoproliferative disorders, type II and III known as mixed cryoglobulinemia, are associated with hepatitis C virus infection and autoimmune diseases. Clinical manifestations are related with occlusion of small and medium blood vessels common in type I cryoglobulinemia while immune-mediated vasculitis is frequent in mixed cryoglobulinemia. Cutaneous damage is the main manifestation, followed by joint, peripheral nerves and renal involvement. We present three cases of cryoglobulinemia that differ from the literature due to their laboratory findings and associated diseases.
References
I. Ferri C. Mixed cryoglobulinaemia. Orphanet J Rare Dis 2008; 3: 25.
II. Wintrobe MM, Buell MV. Hyperproteinemia associated with multiple myeloma. Bull Johns Hopkins Hosp 1933; 52: 156–65.
III. Brouet JC, Clauvel JP, Danon F, et al. Biologic and clinical significance of cryo-globulins. A report of 86 cases. Am J Med 1974;57:775–88.
IV. Trejo O, Ramos-Casals M, García-Carrasco M, et al. Cryoglobulinemia: study of etiologic factors and clinical and immunologic features in 443 patients from a single center. Medicine (Baltimore) 2001;80(4):252-62.
V. Terrier B, Krastinova E, Marie I, et al. Management of noninfectious mixed cryoglobulinemia vasculitis: data from 242 cases included inthe CryoVas survey. Blood 2012;119:5996–6004.
VI. Rieu V, Cohen P, André MH, et al. Characteristics and outcome of 49 patients with symptomatic cryoglobulinaemia. Rheumatology (Oxford) 2002; 41: 290–300.
VII. Sansonno D, Dammacco F. Hepatitis C virus, cryoglobulinaemia, and vasculitis: immune complex relations. Lancet Infect Dis. 2005;5(4):227-36.
VIII. Ferri C, Zignego AL, Pileri SA. Cryoglobulins. J Clin Pathol. 2002;55(1):4-13.
IX. Ramos-Casals M, Stone JH, Cid MC, Bosch X. The cryoglobulinaemias. Lancet. 2012;379(9813):348-60.
X. Ferri C, Sebastiani M, Giuggioli D, et al. Mixed cryoglobulinaemia: demographic, clinical, and serologic features and survival in 231 patients. Semin Arthritis Rheum 2004; 33: 355–74.
XI. Cacoub P, Saadoun D, Limal N, et al. Hepatitis C virus infection and mixed cryoglobulinaemia vasculitis: a review of neurological complications. AIDS. 2005;19 Suppl 3:S128-34.
XII. Cacoub P, Comarmond C, Domont F, et al. Cryoglobulinemia Vasculitis. Am J Med. 2015;128(9):950-5.
XIII. Desbois AC, Cacoub P, Saadoun D. Cryoglobulinemia: An update in 2019. Joint Bone Spine. 2019;86(6):707-713.
XIV. Ferri C, Mannini L, Bartoli V, et al. Blood viscosity and filtration abnormalities in mixed cryoglobulinemia patients. Clin Exp Rheumatol. 1990;8(3):271-81.
XV. Chung L, Funke AA, Chakravarty EF, et al. Successful use of rituximab for cutaneous vasculitis. Arch Dermatol. 2006;142:1407-1410.
Downloads
Published
Issue
Section
License
Copyright (c) 2021 Argentine Society of Dermatology

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor