Herpes zoster. Management and treatment update
DOI:
https://doi.org/10.47196/da.v27i2.2116Keywords:
herpes zoster, diagnosis, treatment, hospitalization, complicationsAbstract
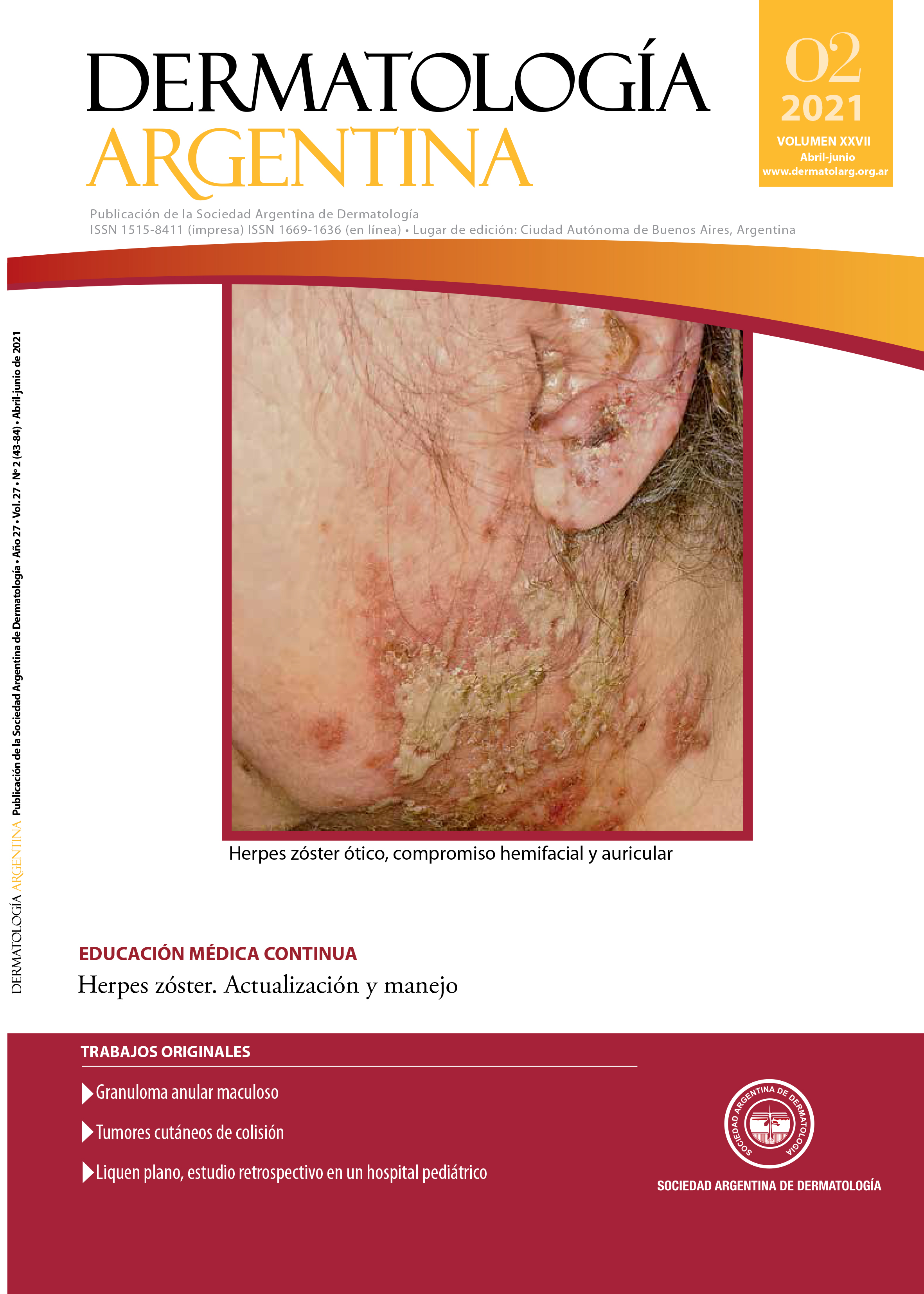
Herpes zoster is an infectious disease caused by varicella zoster virus, characterized by the development of vesicles, which usually present with a metameric arrangement. Its incidence is increasing and is a frequent reason for consultation in daily practice. This article offers updated information on its diagnosis, treatment and prevention, as well as controversial aspects of the management of this pathology.
References
I. Gross GE, Eisert L, Doerr HW, et ál. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia. J Dtsch Dermatol Ges. 2020;18:55-78.
II. Werner RN, Nikkels AF, Marinović B, et ál. European consensus-based (S2k) Guideline on the Management of Herpes Zoster – guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV), Part 1: Diagnosis. J Eur Acad Dermatol Venereol. 2017;31:9-19.
III. Dayan RR, Peleg R. Herpes zoster -typical and atypical presentations. Postgrad Med. 2017;129:567-571.
IV. Schmader K. Herpes zoster. Ann Intern Med. 2018;169:19-31.
V. Chen SY, Suaya JA, Li Q, et ál. Incidence of herpes zoster in patients with altered immune function. Infection. 2014;42:325-34.
VI. Bianchi M, Santiso G, Lehmann E, et ál. Utilidad del citodiagnóstico de Tzanck en un hospital de enfermedades infecciosas de la ciudad de Buenos Aires. Dermatol Argent. 2012;18:42-46.
VII. Dooling KL, Guo A, Patel M, et ál. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108.
VIII. Weber JD, Hirsch MS, Mitty J. Prevention and control of varicella-zoster virus in hospitals. [en línea]. UpToDate, 14 de enero de 2020. Disponible en: https://www.uptodate.com/contents/prevention-and-control-of-varicella-zoster-virus-in-hospitals. [Consultado enero 2021].
IX. Ahronowitz I, Fox LP. Herpes zoster in hospitalized adults: Practice gaps, new evidence, and remaining questions. J Am Acad Dermatol. 2018;78:223-230.
X. Chovatiya R, Silverberg JI. Association of herpes zoster and chronic inflammatory skin disease in US in patients. J Am Acad Dermatol. 2020;1-10.
XI. Preventing Varicella-Zoster Virus (VZV) Transmission from Herpes Zoster in Healthcare Settings, [en línea]. CDC, 14 de agosto de 2019. Disponible en: https://www.cdc.gov/shingles/hcp/hc-settings.html [Consultado enero 2021].
XII. Müllegger RR, Häring NS, Glatz M. Skin infections in pregnancy. Clin Dermatol. 2016;34:368-377.
XIII. Schafer R, Davis M, Phillippi JC. Herpes zoster in pregnancy. J Midwifery Womens Health. 2019;64:230-235.
XIV. Aktaş H, Erdal SA, Güvenç U. Herpes zoster in children: evaluation of the sixty cases. Dermatol Ther. 2019;32:1-5.
XV. Feder HM, Hoss DM. Herpes zoster in otherwise healthy children. Pediatr Infect Dis J. 2004;23:451-457.
XVI. Leung AKC, Robson WLM, Leong AG. Herpes zoster in childhood. J Pediatr Health Care. 2006;20:300-303.
XVII. Comité de Medicamentos. Pediamecum. Aciclovir. Aeped. [en línea], 8 de abril de 2015. Disponible en: https://www.aeped.es/comite-medicamentos/pediamecum/aciclovir. [Consultado enero 2021].
XVIII. Acyclovir (systemic): Pediatric drug information, [en línea], UpToDate. Disponible en: https://www.uptodate.com/contents/acyclovir-systemic-pediatric-drug-information?search=aciclovir [Consultado enero 2021].
XIX. Agentes antivirales. CIME [en línea], 1 de marzo de 2001. Disponible en: https://www.garrahan.gov.ar/PDFS/cime/marzo01.pdf [Consultado enero 2021].
XX. Kakourou T, Theodoridou M, Mostrou, Syriopoulou V, et ál. Herpes zoster in children. J Am Acad Dermatol. 1998;39:207-210.
XXI. Lee HL, Yeoa M, Choi GH, et ál. Clinical characteristics of headache or facial pain prior to the development of acute herpes zoster of the head. Clin Neurol Neurosurg. 2017;152:90-94.
XXII. Wagner G, Klinge H, Sachse M. Ramsay Hunt syndrome. J Dtsch Dermatol Ges. 2012;10:238-244.
XXIII. Jeon Y, Lee H. Ramsay Hunt syndrome. J Dent Anesth Pain Med. 2018;18:333-337.
XXIV. Orgaz Gallego MP, Curbelo del Bosco JM, Tricio Armero MA, Pérez Sánchez S. Un paciente con síndrome de Ramsay Hunt. A propósito de un caso. Rev Clínica Med Fam. 2016;9:119-122.
XXV. Murakami S, Hato N, Horiuchi J, Honda N, et ál. Treatment of Ramsay Hunt syndrome with acyclovir-prednisone: significance of early diagnosis and treatment. Ann Neurol. 1997;41:353-357.
XXVI. Palmerín Donoso A, Tejero Mas M, Buitrago Ramírez F. Herpes zóster oftálmico. Atención Primaria. 2019;51:123-124.
XXVII. Seng Boon HK, You Siang N, Jalaluddin J, Norlina R. Herpes zoster keratouveitis with hypopyon and hyphema. Taiwan J Ophthalmol. 2020;10:54-57.
XXVIII. Werner RN, Nikkels AF, Marinovic M, et ál. European consensus-based (S2k) Guideline on the Management of Herpes Zoster – guided by the European Dermatology Forum (EDF) in cooperation with the European Academy of Dermatology and Venereology (EADV), Part 2: Treatment. J Eur Acad Dermatol Venereol. 2017;31:20-29.
XXIX. Nam KH, Jung ES, Park J, Yun SK. A clinical and etiological study of herpes zoster multiplex. [en línea]. J Am Acad Dermatol, 6 de octubre de 2020. Disponible en: https:// doi.org/10.1016/j.jaad.2020.10.011. [Consultado enero 2021].
XXX. Bollea ML, Bollea Garlatti LA, Vacas AS, Torre AC. Características clínicas y evolutivas de una población con herpes zoster diseminado: un estudio de cohorte retrospectivo. Actas Dermosifiliticas. 2017;108:145-152.
XXXI. Shingles Home. For Health Care Professionals. Clinical Overview [en línea] CDC. 31 de mayo de 2020. Disponible en: https://www.cdc.gov/shingles/hcp/clinical-overview.html. [Consultado enero 2021].
XXXII. Cohen JL. Clinical practice: herpes zoster. N Engl J Med. 2013;369:255-263.
XXXIII. Lara Solares A, Mayoral Rojas V, Guillén Núñez MR, et ál. Consenso multidisciplinario de diagnóstico y tratamiento del dolor neuropático periférico y localizado en México. Gac Med Mex. 2019;155:428-435.
XXXIV. Qian J, Macartney K, Heywood AE, et ál. Risk of recurrent herpes zoster in a population-based cohort study of older adults. [en línea]. J Am Acad Dermatol, 29 de junio de 2020. Disponible en: https://doi.org/10.1016/j.jaad.2020.06.1013. [Consultado enero 2021].
XXXV. Cunningham AL, Lal H, Kovac M, et ál. Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 2016;75:1019-1032.
XXXVI. Oxman MN, Levin MJ, Johnson GR, Schmader KE, et ál. A Vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352:2271-2284.
XXXVII. Baumrin E, Van Voorhees A, Garg A, et ál. A systematic review of herpes zoster incidence and consensus recommendations on vaccination in adult patients on systemic therapy for psoriasis or psoriatic arthritis: From the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2019;81:102-110.
XXXVIII. Disposición 1850 de la Administración Nacional de Medicamentos, Alimentos y Tecnología Médica, Ministerio de Salud de la República Argentina. 27 de marzo de 2013 [en línea]. Disponible en: http://www.anmat.gov.ar/boletin_anmat/marzo_2013/Dispo_1850-13.pdf [Consultado julio 2021].
Downloads
Published
Issue
Section
License
Copyright (c) 2021 Dermatología Argentina

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
El/los autor/es tranfieren todos los derechos de autor del manuscrito arriba mencionado a Dermatología Argentina en el caso de que el trabajo sea publicado. El/los autor/es declaran que el artículo es original, que no infringe ningún derecho de propiedad intelectual u otros derechos de terceros, que no se encuentra bajo consideración de otra revista y que no ha sido previamente publicado.
Le solicitamos haga click aquí para imprimir, firmar y enviar por correo postal la transferencia de los derechos de autor